Milena Germon and Ben Desjarlais, from the Independent Socialist Group (US), examine the threat to public health of monkeypox and the woeful response of the health system while it remains under capitalism.
According to the World Health Organization (WHO), COVID-19 has infected over 600 million people worldwide and accounted for over 6 million deaths–although bias and underreporting factors could mean that the data we have is a conservative guess, at best. When the pandemic initially took hold, it became clear that corporate, profit-based healthcare and the U.S. government were not prepared to handle something like COVID-19 with speed and care. Although the U.S. holds some of the most advanced medicine and technology in the world, neither private healthcare companies nor the corporate political parties effectively used those resources: instead, workers were–and still are–left with individualistic solutions, little support, and limited access to treatment/prevention.
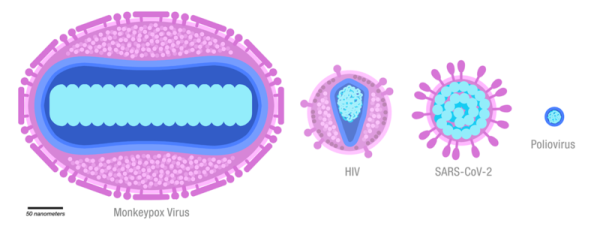
Over two years later, monkeypox has appeared as a major threat to public health–and still, in many ways, it feels like nothing was learned. Monkeypox is most closely related to smallpox and chickenpox and appears with similar symptoms: a flu-ish illness with rash and lesions, some of which can be internal and painful. Though rarely deadly and largely treatable with access to high-quality medicine, monkeypox still poses a severe public health concern as we see outbreaks across the globe.
Monkeypox spreads through direct contact with an infected person and indirect contact with items like clothing. It can also be respiratorily spread through airborne particles. As it stands, the recommended isolation/infection time is between 2 and 4+ weeks, which–as the CDC and other health mega-organizations move towards an unsupportive “hands-off” approach to the COVID-19 pandemic–will prove to be a lengthy and costly recommendation for working people who may not be able to take time off. Not to mention that, because the vaccine response has been staggered, monkeypox is expected to uncontrollably spread once schools open back up without concrete plans and clear guidelines–putting children, teachers, parents, and communities at risk and without a safety net.
Short-term profits prioritised under capitalism
Factually, the health infrastructure in the U.S. is not prepared for or designed to address disease. What makes Monkeypox different from COVID-19 is that there are already two FDA-approved vaccines (JYNNEOS and ACAM2000) since it comes from a familiar family of infections. But that, unfortunately, doesn’t mean that the federal response will be different. Capitalism does not allow for long-term preparation because it only prioritizes short-term profits.
For example, the U.S. stockpiled millions of doses of smallpox vaccines in the early 2000s as a reaction to the perceived threat of bioterrorism. Smallpox was publicly declared “eradicated” in 1980, but the terrorist attacks of 9/11 followed by incidents of anthrax being sent through the mail pushed the U.S. to hoard smallpox vaccines for fear of the disease being weaponized. However, because it was considered too expensive and low-priority to consistently maintain, the government let over 20 million vaccines simply expire. If the stock of smallpox vaccines had been maintained, they could have been used to help prevent the spread of closely-related monkeypox, but instead, there are not enough vaccines to effectively meet the needs of the outbreak.
Due to the lack of a clear and serious response, there’s already a massive amount of misinformation about Monkeypox and who it can affect. In practice, Monkeypox can affect anybody, just as COVID-19 doesn’t discriminate or play favorites. However, because many early U.S. cases appeared in gay men–a demographic more likely to track their health and networks due to the impact of the HIV/AIDs crisis–Monkeypox quickly became labeled as the new “gay disease.” In most places across the U.S., being an MSM (a man who has sex with men) is actually an eligibility requirement for the first wave of Monkeypox vaccinations. And many testing stations have been set up in STI/STD clinics–which, although not wrong, potentially contributes to the developing stigma.
The CDC has done little to combat this reactionary rhetoric. Instead, it explicitly linked community health trends to identity as opposed to high-risk industries like hospitality, service, and education. This linkage is immediately dangerous for LGBT+ people as a whole, but in combination with high transmissibility among children and right-wing anti-queer hysteria, we could also expect a spike in homophobic violence.
It is clear that capitalism is not designed to protect workers. To combat Monkeypox and other infectious diseases, we need to take the drug companies and hospitals under public ownership. By bringing the healthcare system under workers’ control, we could guarantee high-quality, non-discriminatory healthcare to all workers and ensure access to disease screening and life-saving treatments.
